Learning Disabilities and SEND
About SEND
NHS Humber and North Yorkshire Integrated Care Board (ICB) and our partners within Health, the Local Authority, Education and Social Care recognise that children and young people (CYP) are exceptionally important and improving their health and wellbeing is a key priority
The Children and Families Act (2014) places a statutory duty on the NHS to work with local authority partners to provide help and support to children, young people aged 0-25 years, and their families, who have Special Educational Needs and Disabilities (SEND).
SEND covers physical and mental health conditions and learning disabilities: conditions do not have to be long term or lifelong, although many children and young people with SEND do have such conditions.
The Children and Families Act 2014 requires CCGs (ICB’s from July 2022) and health providers, to work effectively together to improve outcomes for disabled children and young people and those with special educational needs (SEND). The aims of this legislation is to ensure a more integrated and personalised service, a focus on outcomes and alignment with a number of key NHS programmes such as Transforming Care (Learning Disability), Child and Adolescent Mental Health Service (CAMHS) transformation and integrated and personalised commissioning.
Our Roles
The Designated Clinical Officer (DCO) role is a key element in supporting health services in the implementation of the Children and Families Act and the scope of the role is very broad. The key responsibilities of the DCO are as follows:
- Oversight – across all health professionals delivering healthcare to individual disabled children, young people and those with special educational needs
- Co-ordination – in relation to the Local Offer, process for mediation arrangements regarding the health elements of the EHC plan and EHC assessments with other key assessments such as Children and Young People’s Continuing Care assessments and Looked After Children Health assessments
- Strategic – contribution to the development of a joint commissioning strategy and participation and engagement strategy.
The Associate Designated Clinical Officer (ADCO) works closely with the Designated Clinical Officer
(DCO) in supporting health services to implement the Children and Families Act (2014). The key responsibilities of the ADCO include:
- Oversight of health advice at the multi-agency EHCP panels
- Providing SEND and EHCP training in relation to health, to health providers and the local authority
- Engaging with partners and stakeholders to ensure the voice of children and young people are at the centre of everything we do
- Provide business support to the DCO (Designated Clinical Officer) and the ADCO (Associated Designated Clinical Officer).
- Act as a first point of contact for colleagues, stakeholders, and multiple external organisations.
- Respond and signpost queries relating to Children and Young people particularly in relation to SEND (Special Educational Needs and Disability).
- Advocate for children and young people with SEND.
Local Offer including SEND specialist support and inclusion
If children and young people aged 0-25yrs have special educational needs and/or a disability (SEND), Your Local Authority Offer will provide them, their families and professionals with accessible information about services and support available locally.
The Local Offer helps you to understand what services you can expect from a range of local agencies, including your statutory entitlements, eligibility and referral criteria. The Local Offer also makes clear what is available from a wide range of services, including:
- Early years settings
- Schools (including academies and free schools) and colleges
- Sport and recreation
- Health services
- Social care
- Employment and further education
Preparing for adulthood
As your child gets older, they may be able to start making their own decisions about a lot of things that matter most to them, this includes their health and wellbeing. Children’s and adult health services are organised differently. If your young person has lots of health needs, there may be many changes to how they receive their health care and support as an adult.
Health teams such as those in your local doctor surgery or hospitals can help them become more independent in managing their own health and moving from children’s health services to adult ones. In healthcare we sometimes call this ‘transition’. Transition can be individualised to meet their needs by clinicians and professional involved. It is important to start thinking about the transition for your child as they move from childhood to adulthood and the services they access. This can be done from the age of 14-18.
You should involve your young person’s GP in planning the transition to adult health services, because they will become more closely involved when your young person turns 18. To find out more visit: 14-25 Transitions Guide.
Transitions can start between 14 to 18 years dependant on the service. This is to ensure adult services are aware of the young persons needs and the transition can be managed in a productive way by the young person, family and professionals. If your child has complex health needs, they should have a named professional in charge of helping their move to adult health services.
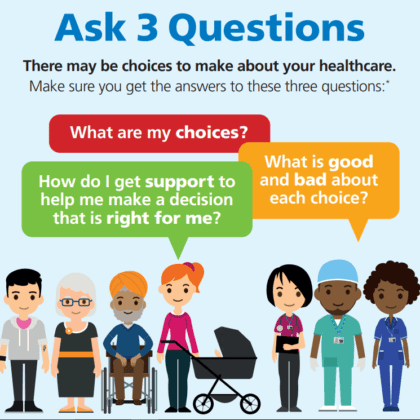
You and your child should be at the centre of the planning process. You should be able to ask questions and give views. The professionals supporting your young person should listen to your views and involve you in decisions about the future. If your child has an education, health and care (EHC) plan their health needs will be recorded as part of their plan. It is important that the professionals who have supported your young person as a child, speak to their colleagues in adult health services in plenty of time. This is to ensure adult staff are fully trained to meet your young person’s health needs and changes to adult equipment and buildings are made.
As you get older, you’re able to start making your own decisions about a lot of things that matter most to you, this includes your health and wellbeing. Health teams such as those in your local doctor surgery or hospitals can help you become more independent in managing your own health and moving from children’s health services to adult ones. In healthcare we sometimes call this ‘transition’. As you move into adulthood you are able to make your own decisions about your health care. This is from 16 years of age. This can sometimes be hard to do but you can ask for help from your parents, a family member, a carer or the National Youth Advocacy service.
National Youth Advocacy Service: 0808 808 1001 help@nyas.net.
Together for short lives is a charity that offers transition support for young people with life limiting or life-threatening conditions. It sets out key standards and goals across healthcare, social care, education, work and housing. Transition planning for these young people may need to acknowledge that their condition may deteriorate, and they may require end of life care. Some young people will have access to specialist paediatric nursing services, home support and residential respite services.
Many of these young people will get NHS continuing care and will be eligible for NHS continuing healthcare for adults. It is very important that health and social care planning for young people with life limiting conditions begins early. Wherever possible children’s and adult health services should overlap. This is to ensure that the transition is as smooth as possible, with new staff gaining experience from existing staff.
I am a young person with SEND
As you get older, you’re able to start making your own decisions about a lot of things that matter most to you, this includes your health and wellbeing. Health teams such as those in your local doctor surgery or hospitals can help you become more independent in managing your own health and moving from children’s health services to adult ones. In healthcare we sometimes call this ‘transition’.
Check out Ready Steady GoClick below for information in other languages:
Annual Health Checks and Health Action Plan
Harshi, her mum Khilna and their GP explain why it is important for people with a learning disability to have an annual health check and to follow a health action plan.
Learning Disability Register

NHS England have developed a leaflet helps people think about whether their child or someone they care for could be considered to have a learning disability and should be on their local GP practice’s Learning Disability Register, to help them get the help they need. You can also access plain English, easy read and accessible versions of the leaflet by clicking here.
Reasonable adjustments
The NHS must make it as easy for disabled people to use health services as it is for people who are not disabled. If you support someone with a physical or mental impairment that has a substantial and long-term adverse effect on their ability to do normal daily activities, please make sure they have good access to healthcare. You can do this by making changes, often quite small, to the way that you care for people. These changes are called reasonable adjustments. Click the button below for further advice.
NHS England: Reasonable Adjustments advice and imagesLiving Well Newsletters
Mental Health Support
For Children and Young People’s Support in North Yorkshire visit our dedicated page or check out The Go-To website. You can find support across the wider Humber and North Yorkshire footprint on Lets Get Better. For adults support, visit this page.
Ask Listen Do – experience support service
Ask Listen Do came from the poor experiences people reported when giving feedback, raising concerns and making complaints. Ask Listen Do resources are designed to:
- make it easier for people, families and paid carers to give feedback, raise concerns and complain.
Please use the following link to understand more about how you can raise your concerns.